Lumbar Epidural Injections
Therapeutic and Diagnostics Benefits for Low Back Pain
A lumbar epidural injection is a safe and effective minimally invasive treatment. This type of spinal injection serves two purposes: (1) reduces nerve inflammation, calms symptoms, aids healing and, (2) provides important diagnostic information.
The procedure involves injecting a local anesthetic and corticosteroid into the epidural space. A corticosteroid is a powerful, slow-releasing, and long-lasting anti-inflammatory medication effective in reducing inflammation. The epidural space is between the protective membrane (dura mater) containing the spinal fluid and the spinal cord, and the bony spinal canal. After the medication is injected, it flows and coats the nerve roots.
There are different approaches to the epidural space: caudal, posterior and foraminal. The foraminal approach is the most direct one for a specific nerve root.
From a diagnostic viewpoint, if the lumbar epidural injection relieves symptoms (i.e. pain), it could mean the nerve targeted is a potential pain generator. Such diagnostic information is beneficial to your doctor for further treatment plan.
Video: Epidural Injections
Click below to view a video from our library about Epidural Injections.
Causes of Low Back Pain
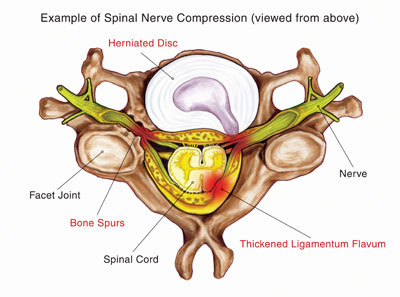
There are many spinal problems that can cause low back pain. As depicted in the illustration, a herniated disc or bone spurs (osteophytes) can compress fragile spinal nerve roots.
Basics about Lumbar Spinal Nerves
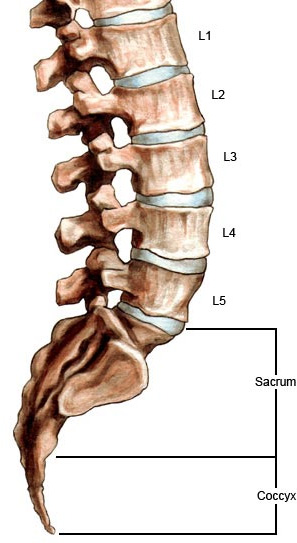
In the lumbar spine there are 5 pairs of spinal nerves. Each pair of nerves provides sensation and function to parts of the body. Just as the levels of the lumbar spine are abbreviated, the spinal nerve pairs are numbered in a corresponding way. The L1 nerve roots exit the left and right sides between the first and second lumbar vertebrae (L1-L2). L5 exits between the last lumbar vertebra and the sacrum (L5-S1).
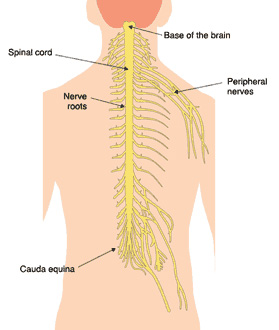
Each pair of nerve roots exits the spinal column and branch out into the body forming the peripheral (outer) nervous system. These nerves innervate the lower part (below the waist) of the body and enable movement (motor function) and feeling (sensory function).
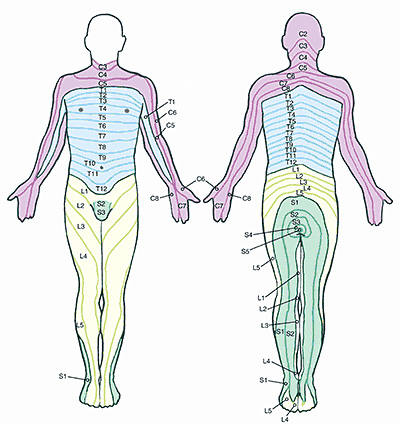
The illustration below depicts this pattern called dermatomes. Your doctor uses the dermatomal pattern of your symptoms to help diagnose the location of your spinal problem based on where you have pain or weakness.
Epidurals by Transforaminal Approach
For a more specific placement, at times a transforaminal approach epidural injection is advised. By bringing the needle a little further from midline to the side, this approach places the needle directly at a single nerve level. A single nerve can be isolated for either diagnostic reasons or to deliver medications into a tight nerve channel (neuroforamina) for better results. Due to arthritis, there may be tightness around the nerve, and an injection by the more traditional approach would not be as effective.
Based on your symptoms, medical history, physical and neurological examination, and imaging study findings (X-ray, MRI), your doctor will determine which spinal nerve root(s) may be generating pain and other symptoms. Then the injection can be better planned for the spine level involved.
Patient Procedure Preparation
In advance of your procedure appointment, our medical team provides you with instructions specific to you and medications you regularly take.
If you take blood-thinning medication, such as Coumadin, Plavix, aspirin, etcetera, please notify our medical team. Certain drugs must be stopped several days before your procedure.
Possible Risks and Complications
A lumbar epidural injection, like other medical procedures, may present risks. Although extremely rare, possible risks or complications include bleeding, infection, nerve injury, and allergic reaction to medication. More common is an increase in pain, injection site tenderness, and steroid side effects.
What to Expect: The Procedure and After
Upon arrival at the treatment facility, our nurses meet you in the preoperative area. If necessary, medications to relax you are given intravenously (IV).
Then you are positioned face down with a cushion under your abdomen to flex the spine and keep you comfortable. Next, the skin area is cleansed with a sterile soap. A local anesthetic is injected and given time to take effect.
Using fluoroscopic guidance (real time x-ray), the doctor proceeds with the procedure and places the needle tip at the target area. The doctor confirms the needle tip is properly positioned visually and fluoroscopically. He then injects a small amount of contrast (dye) to ensure correct spread. Next, a low volume anesthetic / corticosteroid solution is injected. Rarely is pain increased during the injection. However, our medical team is dedicated to making you as comfortable as possible. A small Band-Aid covers the injection site.
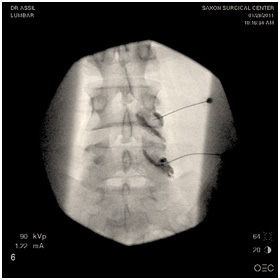

A sample of Dr. Assil's fluoroscopy photos during a lumbar epidural injection procedure
Usually, the procedure takes 15 to 20 minutes. Afterward, in the recovery area, our nurses closely monitor you for about 25 minutes.
Before you are released home, our medical team provides you with written home care instructions. Some patients experience 2 to 3 days of discomfort after the procedure. This is normal and does not necessarily mean the corticosteroid is not taking effect.
Conclusion
A member of our medical team will telephone you 24 to 48 hours after your lumbar epidural injection to follow-up. We recommend you keep a daily journal of your pain level and other symptoms following your procedure. Please be specific and keep in mind where pain and symptoms are in relationship to the injection site. The pain diary will help you provide your doctor with detailed information about your treatment progress when you come back for your follow-up office visit.
Download Epidural Injections Post-Procedure Care Form
You will be provided with specific discharge instructions following your procedure customized to your condition. The attached instructions are provided only as an indication for pre-planning purposes and do not replace or supercede the specific discharge instructions, which will be provided to you by the Recovery Nurse.
Our multidisciplinary pain practice is
interventional and comprehensive.

Some Conditions We Treat
- Herniated Disc
- Peripheral Neuralgia
- Post Laminectomy Syndrome
- Spinal Stenosis
- Spinal Spondylolisthesis

