Radiofrequency (RF) Rhizotomy – RF Neurotomy
Advanced Therapeutic Treatment for Spinal Facet Joint Pain
The purpose of medial branch radiofrequency (RF) rhizotomy, or RF neurotomy, is to reduce or eliminate facet joint pain and related symptoms as related to spine pain due to facet joint inflammation or injury.
-
Upper Neck
In the upper neck (cervical spine), the C2-C3 facet joint is vulnerable to injury and can cause significant upper neck and posterior headaches that refer to the back of the eye. This kind of headache is different from a migraine but, when it flares up, it can trigger a migraine episode. However, it does not respond to migraine medications. -
Lower Neck
In the lower neck, usually C5-C6 is most vulnerable to injury and the cause of chronic neck pain. Pain in this area refers from the mid neck down to the scapular and upper back region. Research shows that other facet joints can also be injured. -
Low Back
In the low back (lumbar spine) facet injuries can occur at any level, but are more common in the lowest two segments: L4 - L5 as well as L5 - S1. Pain from facet injury in the low back usually refers to the buttocks and posterior thighs. It is different from sciatica, as pain is broad and vague. Usually, muscle spasms develop over the painful facet joints.
Video: Lumbar Radiofrequency Neurotomy
Click below to view a video from our library about Lumbar Radiofrequency Neurotomy.
Goal of RF Neurotomy
The goal of the Radiofrequency Neurotomy procedure is to disrupt pain transmission from previously identified painful facet joints. Using the analogy of a dental root canal, the dentist easily identifies the painful tooth. After the tooth?s nerves are disabled, the tooth no longer causes painful sensations. Similarly, when a facet joint?s medial branch nerve is disabled, it no longer causes pain to be felt. These nerves do grow back after 9 months on average.
The facet joints cannot be replaced and surgically fusing the joints may not be indicated. However, when severe pain has not responded to conservative therapies, RF neurotomy may provide pain relief, as well as delay or avoid surgical intervention altogether.
Before RF Neurotomy
Before a RF Neurotomy is performed, the pain generating facet joint(s) has been identified by means of a diagnostic injection, such as a facet joint or medial branch nerve block. Other tests may include MRI or CT scans that are not able to show the location of pain. Since the medial branch nerves do not control major neck or low back muscles, it is relatively safe to disrupt or turn off their ability to send signals to the brain that include pain.
What's Involved?
RF neurotomy is a precisely targeted needle placed to create controlled heat to stun function of the facet joint?s medial branch nerve.
Sophisticated computerized equipment delivers radiofrequency energy to the needle. The needle?s tip is positioned parallel and close to the targeted nerve. Energy is only dissipated from the tip of the needle to neighboring tissue. The resistance of the tissue causes the energy to convert to heat. A probe (a thermo-coupler) within the needle measures the heat. The computer maintains the temperature at a pre-designated setting; usually between 75 to 85-degrees Celsius, which is well below the boiling point.
Only the small internal nerve filaments will degenerate. The side effects, which last up to 4 weeks, are expected and relatively minor. Relief from pain and related symptoms may last 9 to 14 months or longer. However, the small nerve regenerates (grows back) and facet joint pain may come back. We have patients who know exactly when their pain is starting to return and therefore contact us for repeat of the Radiofrequency Neurotomy Procedure.
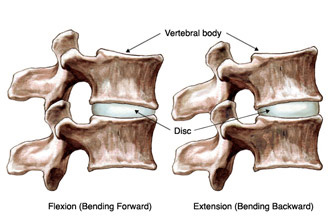
Basic Facet Joint Anatomy
Each vertebra in the cervical (neck), thoracic (chest), and lumbar (low back) has two sets of facet joints at the back of the spine. One pair faces upward and one downward with a joint on the left and right sides of the vertebra. Facet joints are hinge-like and link vertebrae together.
Two medial branch nerves innervate each facet joint, one from above for the upper portion and one from the same spinal level for the lower half of the joint. The medial branch nerves control sensation to the facet joint, and bring input to a small muscle and a small patch of skin in the same area of the back. When there is degeneration or inflammation within a facet joint, pain activates the medial branch nerve. These nerves do not control sensations or movement in your arms or legs.
Patient Procedure Preparation
In advance of your procedure appointment, our medical team provides you with instructions specific to you and medications you regularly take.
If you take blood-thinning medication, such as Coumadin, Plavix, Prodaxa, aspirin, etcetera, please notify our medical team. Certain drugs must be stopped several days before your procedure.
Possible Risks and Complications
A radiofrequency neurotomy, like other medical procedures, may present risks. Complications include risk of infection, low blood pressure, headache, and allergic reaction to medication.
The expected side effects include sensation of sunburn on a small area of the skin where a branch from the nerve provides input. With the procedure in the upper neck, there may be difficulty with balance, usually seen in older patients. These symptoms may last 3 to 4 weeks.
What to Expect: The Procedure and After
Upon arrival at the treatment facility, our nurses meet you in the preoperative area. If necessary, medications to relax you are given intravenously (IV). If IV sedation is administered, you will be relaxed and may not remember most events. However, you can be roused during the procedure. At specific times, it is important for Dr. Assil to know how you are feeling.
In the operating room, you are comfortably positioned and a cushion is placed either under your chest or abdomen, depending on the area of the spine targeted. Next, the skin area is cleaned with sterile soap. A local anesthetic is injected and given time to take effect.
Using fluoroscopic guidance (real time x-ray), the doctor precisely positions the special needle. The needle is Teflon-coated, except at the last one-centimeter (10mm) where the exposed tip is positioned beside the targeted medial branch nerve.
The position of the needle is confirmed visually in different views, oblique, back to front, and from the side. Next, for physiological confirmation, the needle tip is stimulated using very low current at specific frequencies. This tests the closeness of the needle tip to the targeted nerve and ensures it is at a safe distance from the larger segmental nerves. Then, by means of the thermo-coupler electrode, radiofrequency energy is delivered and the temperature in the surrounding tissue is measured. As the tissue next to the needle is heated, the medial branch nerve is stunned or rendered ineffective.
Throughout the procedure, our medical team is dedicated to making you as comfortable as possible. After the procedure, small adhesive bandage covers the injection site.

A sample of Dr. Assil's fluoroscopy photo during cervical RF neurotomy
Depending on the number of spinal levels injected (usually 2 to 3); the procedure takes approximately 45-60 minutes. Afterward, in the recovery area, you are closely monitored. Before you are released home, our medical team provides you with written home care instructions.
Download Radiofrequency Post-Procedure Care Form
You will be provided with specific discharge instructions following your procedure customized to your condition. The attached instructions are provided only as an indication for pre-planning purposes and do not replace or supercede the specific discharge instructions, which will be provided to you by the Recovery Nurse.
Our multidisciplinary pain practice is
interventional and comprehensive.

Some Conditions We Treat
- Herniated Disc
- Peripheral Neuralgia
- Post Laminectomy Syndrome
- Spinal Stenosis
- Spinal Spondylolisthesis

